
Sara Skoog started college as pre-med, switched her major to English and has spent 20+ years writing about medical education and health care. Hobbies include baking, crosswords and not watching sports.
Author Page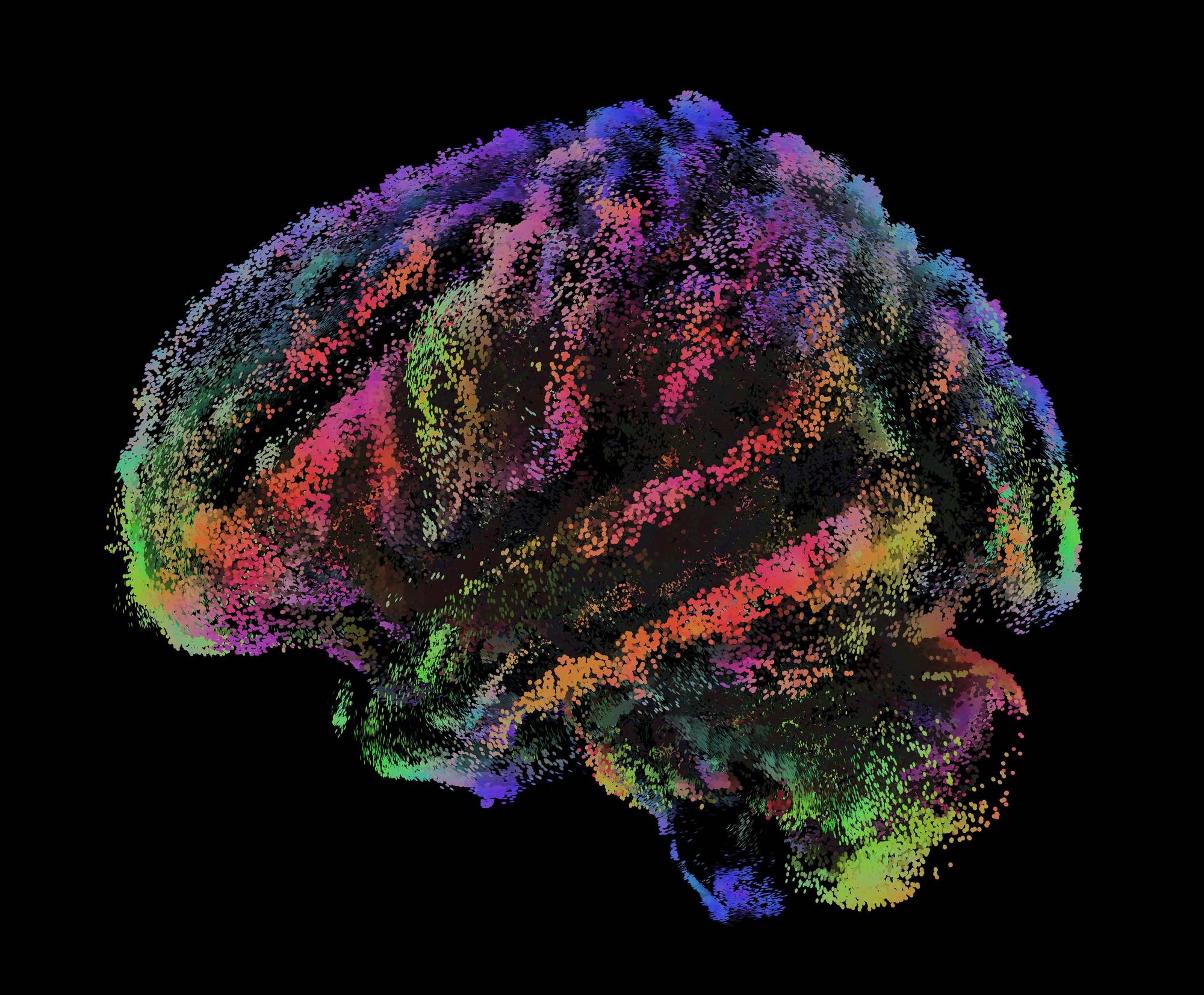
Neural Constellations:
Connecting the Dots
This image presents a sagittal view of the endpoints of 100 million axonal pathways in the human brain. It offers a state-of-the-art depiction of the brain’s complex structural connectivity, illuminating how regions work together to support cognition, perception and behavior in health and disease. Its creator, Shawn Flanagan, PhD, sees this visualization as an artistic celebration of the brain’s intricate design and a tribute to the study of neural connections. Dr. Flanagan is an associate professor in the Dr. William M. Scholl College of Podiatric Medicine and director of the Human Performance Laboratory in the Center for Lower Extremity Ambulatory Research (CLEAR).
It’s everywhere. At home, at work, at school, on our TVs and phones. We don’t always know stress when we see it, but we know when we feel it. The stress response occurs without conscious effort. It happens, and our bodies are just along for the ride. The pulse races, muscles tense — do you fight? Take flight? Or freeze?
The body does what the brain tells it to do, a sort of autopilot that prioritizes essential functions in an effort to get all systems back on the level. The stress response exists to keep us safe in the moment, but too much stress takes its toll. What exactly is happening in the brain, and why do we react the way we do?
“Primary regions of the brain involved in the initiation of the stress response are the amygdala, hippocampus and cortex,” says Janice Urban, PhD, professor and director of RFU’s Center for Neurobiology of Stress Resilience and Psychiatric Disorders, an expert on how stress affects the brain. “These regions are responsible for recognizing sensory input. When we confront a perceived stress — something we see, smell or hear — these brain regions are activated and send signals to the rest of the body to assess whether this is something we need to worry about.”
The way the body recognizes and responds to stress comprises three stages: alarm, resistance and exhaustion. The sensory processing Dr. Urban describes begins the alarm stage, which includes the sensations most of us associate with stress.
“These sensory signals filter to the hypothalamus, which is sometimes called the reptilian part of the brain — the hormonal part of the brain,” Dr. Urban explains. “The hypothalamus releases stress hormones, such as cortisol, and activates the autonomic nervous system, which releases adrenaline and also regulates breathing and heart rate. The body mobilizes all its efforts to support processes important for survival.”
Stress can be acute or chronic. An acute stress response happens over a short period of time. Say you’re afraid of dogs and come across one while walking down the street. In a matter of seconds, your body tells you how to respond. You run away, or freeze until the dog walks away, and then it’s over. Your brain gives the “all clear,” and systems return to normal functioning. Acute responses can be good for survival, steering you away from real or perceived immediate danger. Chronic stress results when the stress response is activated over long periods of time. It can manifest as cardiovascular issues, sleep disruption, weakened immune function, gastrointestinal upset, depression and anxiety. This leads into the final stage, exhaustion, when the body can no longer put up resistance to stress, and chronic health conditions can worsen if left untreated.
The evidence linking stress with physiological and psychological symptoms is well established. But what does stress do to the brain itself? Does it reset, or is it permanently altered?
“That’s the million-dollar question: We assume that, after acute stress, things return close to normal — maybe right away, or in a few days depending on the stressor,” Dr. Urban says. “Some of the effects of chronic stress can persist, resulting in mood disorders and deficits in memory and learning. Maybe these are long-term changes that you can recoup, or maybe not.”
Dr. Urban and her colleagues are working to better understand the specific neural circuits that drive normal behaviors, and how fear, social stressors, pain and illness affect how these circuits function. Since not all stressors affect the brain the same way, their collective work is key to identifying important processes or mechanisms as potential targets for treating, or even preventing, stress-related illnesses.
Advance world-class research and innovation to improve patient lives and well-being.